No risk of infection
HIV cannot be transmitted during everyday activities because saliva, sweat, tears, urine or faeces do not contain enough of the virus to cause infection - not even in HIV-positive people who are not receiving HIV treatment. Intact skin is a safe barrier, so HIV cannot be transmitted through unbroken skin. HIV also cannot survive for long periods of time outside the body.
Therefore, there is no risk of infection in the following situations:
Being coughed or sneezed on
Hugging or kissing (even if there are small wounds in the mouth)
Insect bites (HIV cannot survive in the digestive tract of mosquitoes)
Sharing plates, glasses and cutlery
Shared use of toilets, towels or bed linens
Visiting swimming pools or saunas
Working and/or living together
Caregiving and nursing
As long as the standard hygiene regulations (e.g. use of disposable materials and sterile instruments) are observed, there is no risk of infection during:
First aid
Medical treatments, such as dental treatment or surgical procedures
Cosmetic treatments, such as hand and foot care
Tattooing and piercing
In these situations, it is also not necessary to use special protective equipment, or only give HIV-positive people appointments at the end of the day in order to facilitate thorough cleaning and disinfection of the treatment room after treating an HIV-positive person.
If you have been discriminated against in public because of your HIV infection—for example in hospital, when visiting a doctor, at work or with a public authority—you can report this to the HIV-related discrimination contact centre.
Possible high-risk situations
HIV is always transmitted through the exchange of body fluids that contain a particularly high amount of HIV. Body fluids that may contain sufficient amounts of HIV include:
Blood
Semen
Vaginal fluid
Fluid film on mucous membranes
(for example, penile mucosa, intestinal mucosa, vaginal mucosa)
Breast milk
There is not enough HIV for transmission in other body fluids, such as saliva or sweat.
In the following situations, there is an increased risk of acquiring HIV:
Unprotected vaginal intercourse or anal sex
Unprotected oral sex if menstrual blood or semen enters the mouth
Sharing contaminated syringes, such as in the case of intravenous drug use
Occupational exposure, such as a needle injury
In all cases, the following applies: there is only a risk of infection if if the donor/sex partner was not receiving HIV treatment and had a detectable viral load.
If, on the other hand, an HIV-positive person receives HIV therapy that reduces the number of viruses to such an extent that no more viruses can be detected in the blood using standard methods, then there is no risk of HIV transmission in the situations just mentioned.1, 2
This also applies in the case of pregnancy. Without successful HIV treatment, there is a risk that an HIV-positive mother will transmit HIV to her child during birth. However, if the expectant mother receives HIV treatment that is so successful that her viral load is undetectable then she cannot transmit HIV to her child during the pregnancy, at birth or through breastfeeding. For more detailed information about HIV and pregnancy, see the section “HIV-positive and pregnant“.
Post-exposure prophylaxis (PEP)
If a high-risk exposure has occurred, it is still possible to prevent infection with HIV: post-exposure prophylaxis (PEP). PEP is a four-week medical treatment that can prevent the HIV virus from taking hold in the body. Successful PEP ensures that exposure to HIV does not lead to infection.
- To use PEP to prevent a possible infection, action must be taken quickly: It is important to see a doctor as soon as possible after the high-risk contact, because PEP should be initiated within 24 hours, ideally within 2 hours after the high-risk contact. If more than 72 hours have passed since the high-risk contact, PEP is usually no longer effective.
A doctor can also provide more accurate advice about whether PEP is necessary in your specific situation or not. Since PEP, like any medical treatment, can have undesirable effects, its use should be limited to true emergencies. If there is no doubt that the high risk exposure was with a person known There is no doubt that the high risk exposure was with a person known to be HIV-positive and is not receiving HIV treatment: In this case, PEP should always be administered. If it is uncertain whether the person is HIV-positive or negative, the risk of transmission will depend on the type of contact. If you are unsure: ask a doctor – if in doubt, it’s better to take it even if you do not need it!
Viral load and detection limit
The viral load is the amount of HIV measured in the blood. If the viral load is high, it means that there is a lot of HIV in the blood. These viral particles can then infect other cells and therefore spread further in the body. The following applies: the higher the viral load, the faster the infection can progress and the higher the risk of transmitting the virus in certain situations.
With the right treatment, it is possible to stop HIV from multiplying, so that the viral load decreases. Treatment is considered successful when the viral load is reduced below the “detection limit”. This term refers to the limit below which HIV can no longer be detected in the blood using the latest measurement methods available.
- The level at which HIV can be detected in the blood in a specific case depends, among other things, on which measuring method and which measuring device is used in the laboratory. In order to enable uniform treatment of HIV regardless of the actual measurement method used, the treatment guidelines for doctors treating HIV define a value of approx. 40–50 virus copies per millilitre of blood (abbreviated c/ml) as the detection limit.2, 3 The doctor therefore speaks of non-detectability of the HIV virus if the number of HIV viruses in the blood is less than 50 virus copies per millilitre of blood.
In recent years, a number of scientific studies have been conducted on the question how likely HIV transmission can occur whilst receiving successful treatment. The most important studies in this regard were the PARTNER studies.4, 5 Two large studies examined whether HIV transmission occurs through condomless-sex in couples where one partner is HIV negative and the other partner is HIV positive. The results of these studies showed that there was no HIV transmission if the HIV-positive partner was permanently below the detection limit due to HIV treatment. In these studies, a viral load of less than 200 virus copies per millilitre of blood was even considered the detection limit and achieving this value was therefore considered a successful treatment. To be on the safe side, medical guidelines recommend that the goal of successful HIV treatment is an even greater reduction in the viral load: Detection limit < 50 virus copies per millilitre of blood.
If you are HIV-positive, you cannot transmit HIV even if you have sex without a condom as long as you are receiving effective HIV therapy: this knowledge is important for everyone – regardless of their HIV status.
However, it is crucial that the medications are taken consistently and correctly. This is the only way to keep the viral load below the detection limit permanently. If HIV medication is taken irregularly, there is a risk that the viral load will increase again and resistance to the medications may develop. Through resistance HIV drugs may lose their efficacy.
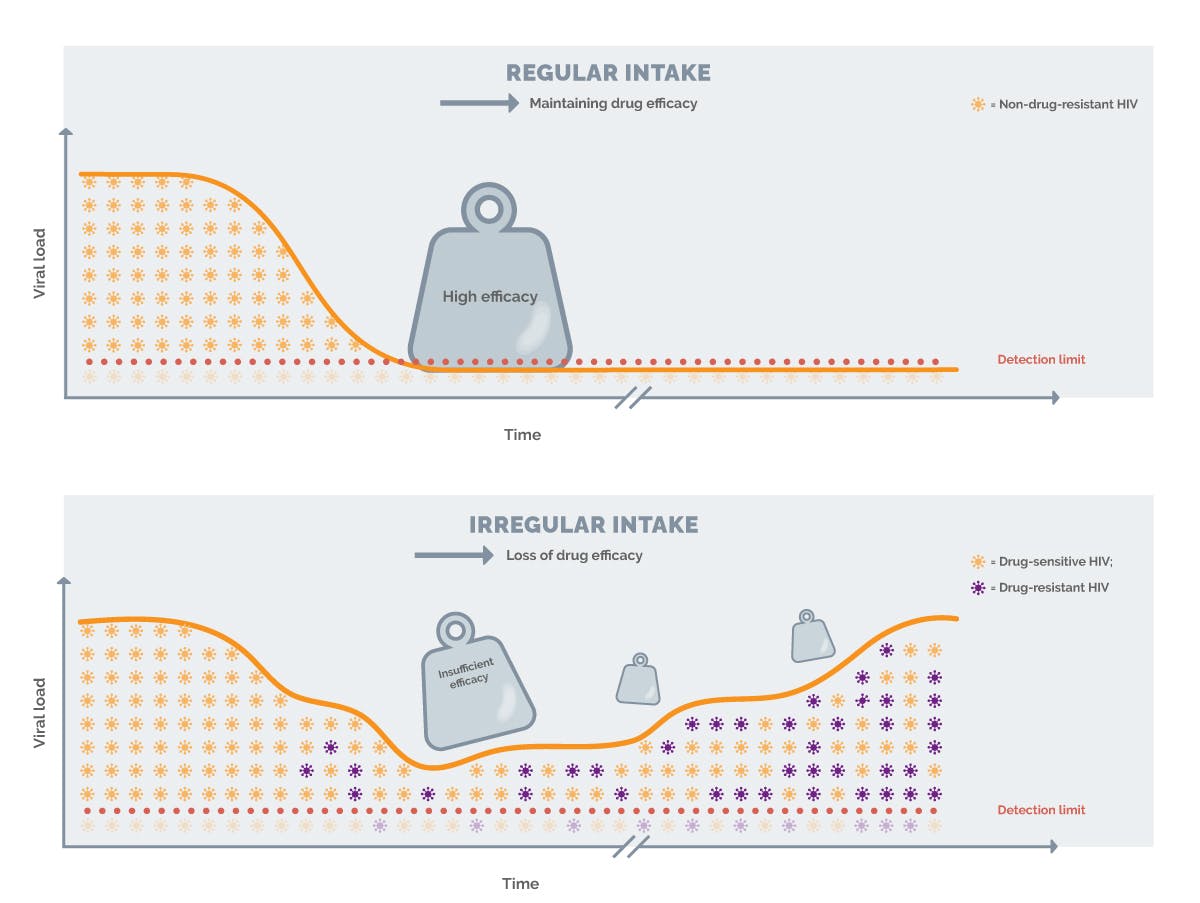
Image: Schematic representation of the effects of regular intake of HIV medication on treatment success compared to irregular use
Further information on taking medication regularly can be found in the section "Adherence to treatment“.
PREVENTIVE MEASURES
HOW TRANSMISSION OF THE VIRUS CAN BE AVOIDED
If you recall the prevention campaigns of previous years, it becomes clear: for a long time, condoms were considered the only effective measure for protecting against HIV infection. In the meantime, there has been a change: In addition to condoms, so-called “prevention through treatment” and pre-exposureprophylaxis (PrEP) – not to be confused with post-exposure prophylaxis (PEP) – are recognised as effective preventive measures.
Below you will find more detailed information on the three most important ways to prevent infection with HIV:
Condoms
HIV is most commonly transmitted through condomless sexual intercourse. The use of condoms prevents this. The variant for women, the femidom, can also protect against HIV. In both cases, sperm or vaginal fluid is prevented from coming into contact with mucous membranes. This can protect against HIV, as well as other sexually transmitted diseases.
Treatment Prevention
Unfortunately, even today, HIV infection is not curable. However, thanks to intensive research and modern forms of treatment, people with HIV can now live long and healthy lives. The progression of the infection to the clinical profile of AIDS can also be prevented. Another major benefit of modern HIV treatment is the ability to suppress HIV to such an extent that there is no risk of transmitting the virus to others. This happens when the number of viruses in the blood is reduced so much that it is permanently below the “detection limit“..1, 2
However, this requires that appropriate HIV treatment is started in time and adhered to. If the virus is permanently below the detection limit due to successful HIV treatment, HIV can no longer be transmitted, even during sex without a condom1, 2 – which is another important step towards a normal life for people with HIV and their partners. By permanently reducing the viral load below the detection limit, we can achieve "prevention through treatment" or a status of “U=U” ("undetectable = untransmittable").
PrEP stands for "pre-exposure prophylaxis". This means taking medication as a precaution to protect yourself from infection with HIV. Anyone who is at increased risk of a possible HIV infection can be prescribed PrEP upon request. Prescription is issued by a doctor who specialises or with experience on the treatment and prevention of HIV on the treatment of HIV. A list of these doctors is available online at DAGNÄ website (German Association of General Practitioners Caring for HIV-Infected Patients).
In many cases, the costs for these medications are covered by statutory health insurance, while private health insurance companies usually have their own regulations. PrEP is usually taken daily. However, there is also the event-based, in which the medication is taken at specific intervals before and after sex. Important note: PrEP only protects against HIV if it is taken as prescribed. However, PrEP does not protect against other sexually transmitted diseases.
References:
- Eisinger RW et al. HIV Viral Load and Transmissibility of HIV Infection: Undetectable Equals Untransmittable. JAMA 2019 Feb 5; 321(5): 451–452.
- Leitlinien der European AIDS Clinical Society (EACS), Version 12.0, last updated October 2023. https://www.eacsociety.org/guidelines/eacs-guidelines/eacs-guidelines.html.
- Guidelines for diagnosis and treatment of HIV infection of the German AIDS Society (DAIG). German-Austrian guidelines. Last updated September 2020. https://daignet.de/site-content/hiv-leitlinien/hiv-leitlinien
- Rodger AJ, Cambiano V, Bruun T et al. Sexual Activity Without Condoms and Risk of HIV Transmission in Serodifferent Couples When the HIV-Positive Partner Is Using Suppressive Antiretroviral Therapy. JAMA 2016, 316(2): 171–181.
- Rodger AJ, Cambiano V, Bruun T et al. Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): final results of a multicentre, pro- spective, observational study. Lancet 2019; 393(10189): 2428–2438.
NP-DE-HVU-WCNT-250003 – February 2025