Discovery
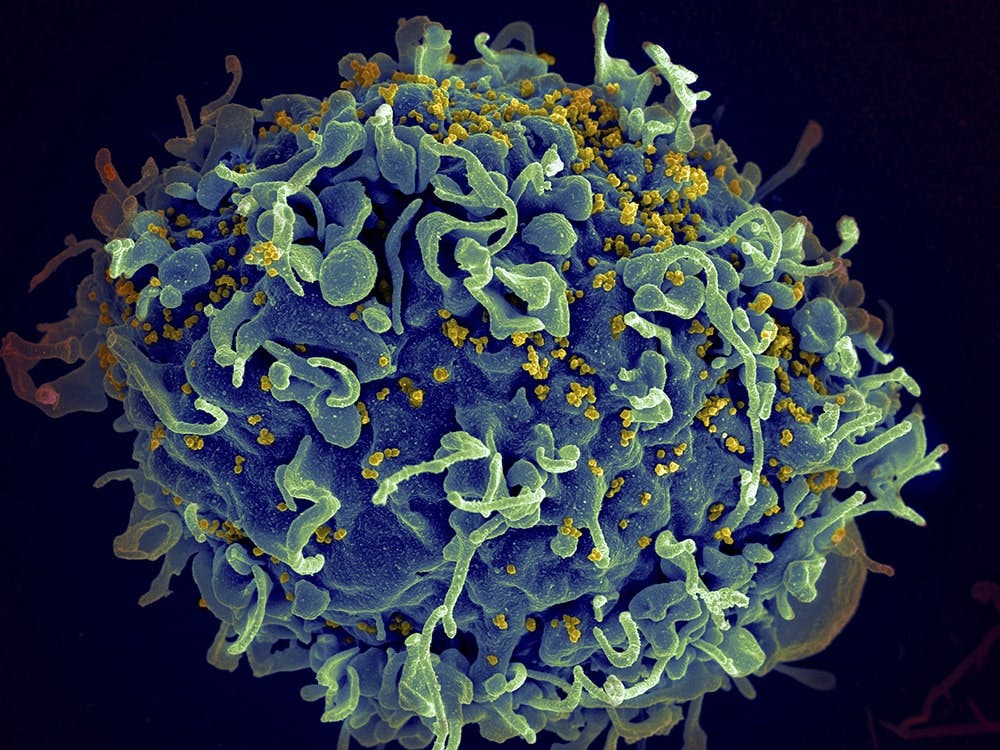
It is not possible to say with certainty when the HIV virus first appeared. In the US, HIV Transmission began in the early 1980s. At that time, an otherwise rare form of pneumonia, caused by a general weakening of the immune system, was becoming more common. The trigger for this mysterious immune system deficiency, soon to be known as Acquired Immune Deficiency Syndrome (AIDS), was a new virus identified in 1983. In that year, the French researcher Luc Montagnier succeeded in isolating the virus and observing it under the electron microscope, and a few months later, US researcher Robert Gallo followed suit.1 In 1986, the new virus was given the name human immunodeficiency virus (HIV). It is now believed that the HIV virus originated in wild monkeys in Central Africa. In a way that is not yet fully understood, the virus was transmitted to humans and then around the world.
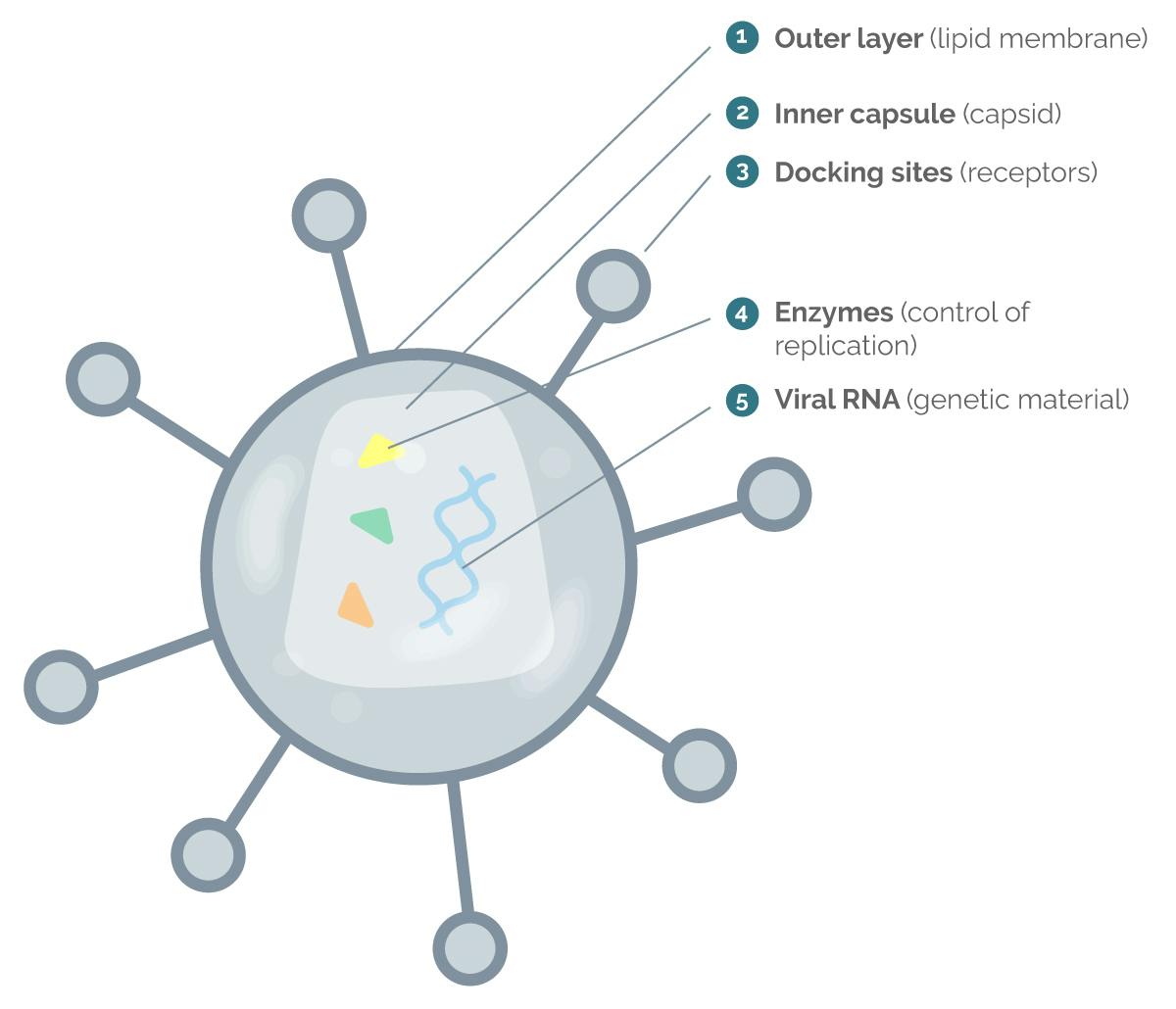
Structure of the HIV virus
The HIV virus consists of an outer shell (lipid membrane) and an inner capsule (capsid). There are docking sites on the shell that help it to dock onto a human cell (host cell). The inner capsule contains the blueprint of the virus, also known as genetic material or viral ribonucleic acid (RNA ), as well as various enzymes. These enzymes serve as tools for the replication of the HIV virus within a human immune cell.
Target cells
The abbreviation "HIV" stands for Human immunodeficiency virus. The name reveals which cells the virus targets: the cells of the human immune system – specifically the cells that protect the body from pathogens such as bacteria or viruses.
The functioning of the immune system is based on a complex interaction of different groups of immune cells:
- CD4 helper cells: a kind of "operations hub" that coordinates the immune response by activating other cells of the immune system.
- B cells: a kind of "search service" that finds pathogens and marks them with the help of antibodies so that they can then be recognised and eliminated by other cells of the immune system
- CD8 killer cells: a kind of "special unit" that can directly attack and eliminate intruders such as bacteria or viruses
Course of the infections
Infection of human cells with the HIV virus occurs in the following steps:
The virus docks via receptors on the surface of immune cells (mainly CD4 helper cells).

The virus connects with the cell (fusion) and introduces its genetic information and various enzymes.

Using the enzyme reverse transcriptase, the HIV virus adapts its genetic material (viral RNA) to that of the human cell (DNA).

Another enzyme, the integrase, incorporates the virus's adapted genetic material into the human genetic material.

Human cells now produce individual virus components that can combine to form new HIV viruses.

These new virions protrude from the human immune cell, detach themselves from it and enter the blood.

The finished (mature) virus is now in the bloodstream and can infect other cells again.
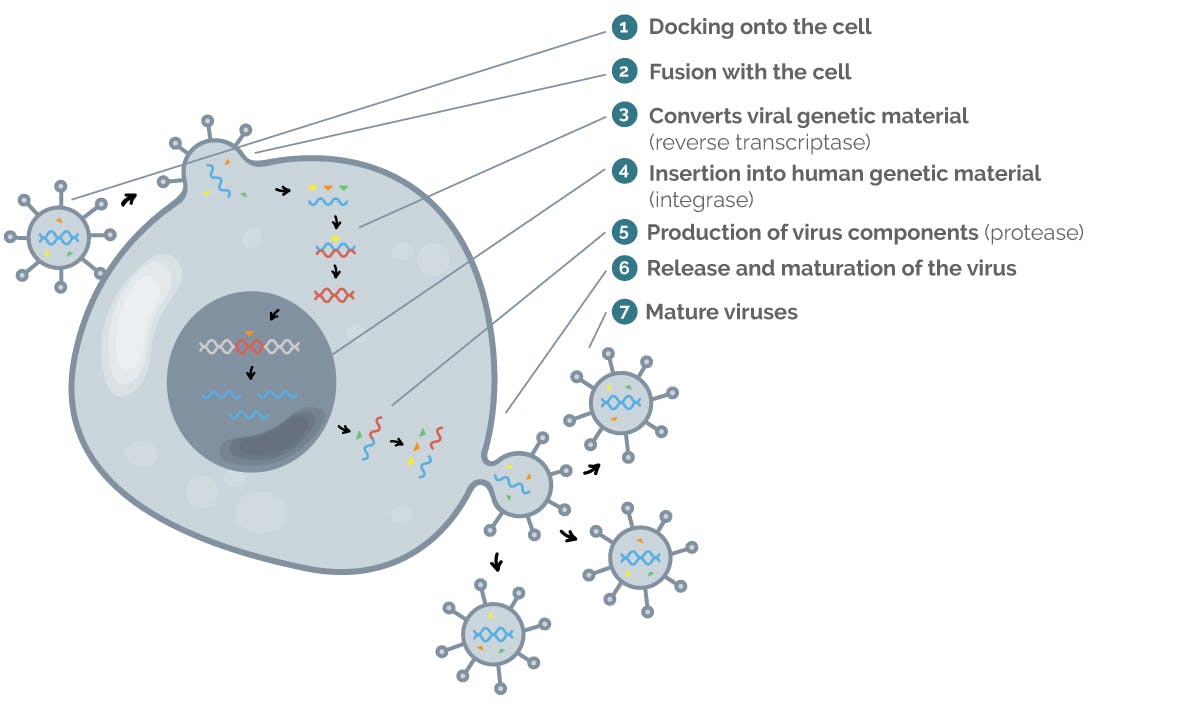
Image: Schematic representation of the spread of HIV
So-called antiviral age nts, i.e. substances that act specifically against viruses, can intervene at various stages of this process and interrupt the production of new viruses. For example, there are inhibitors that bind to the enzyme integrase (position 4 in the image). They disrupt the incorporation of the viral genetic material into the DNA of the human cell and thus interrupt the replication of the HIV viruses.
For more detailed information on how HIV medications work and how they stop HIV viruses from replicating, see the chapter “HIV treatment“.
Phases of HIV infection
If an HIV infection is not treated with medication, the viruses can continue to replicate in the body and weaken the immune system to such an extent that AIDS develops. However, modern therapies make it possible to stop this process. People with HIV can therefore lead normal, long lives if they take their HIV medication regularly.
HIV infection occurs in three phases:
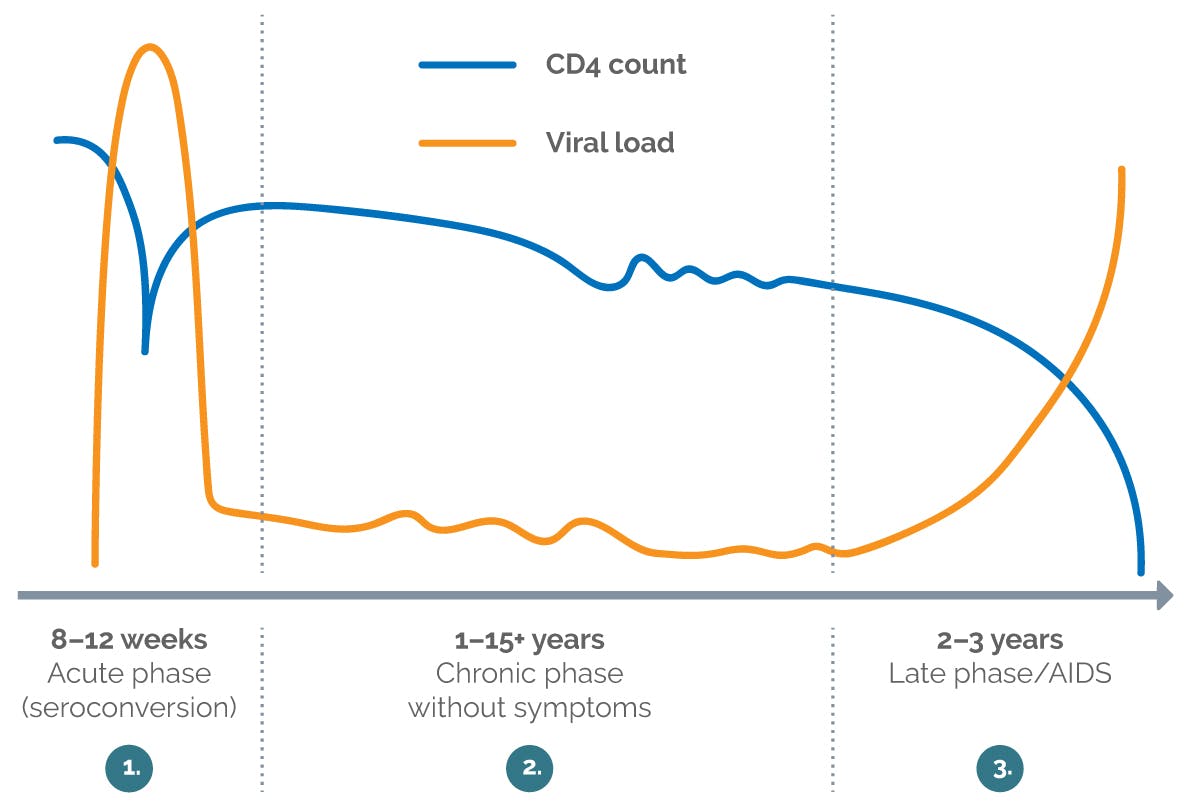
Image : Progression of viral load and CD4 cells in an untreated HIV infection (modified after Rowland-Jones 20032)

Acute phase:
Immediately after infection, the viral load, i.e. the amount of HIV in the blood, increases very quickly. The HIV virus replicates in certain cells of the immune system, known as CD4 cells, which are then destroyed. The number of these cells, which are important for immune defence, therefore drops significantly immediately after HIV infection.
A few weeks after the infection, antibodies against the HIV virus have formed in the blood (the doctor calls this process seroconversion), so that the HIV infection can now be detected by a test. In the acute phase, with its rapid increase in viral load, the risk of the virus being transmitted to other people, for example through condomless sexual intercourse, is particularly high. This is especially critical when an HIV positive person is unaware of their HIV statusdoes not yet know about his or her infection.
The immune system recognises the HIV virus as a foreign particle and tries to prevent it from replicating. Flu-like symptoms such as drowsiness, fatigue or fever often occur, but these disappear after a while. As the immune systems begin to identify the virus, the viral load usually drops again, but only to some extent. A certain amount of viruses still remain in the blood.

Chronic phase:
Over a period of time—sometimes even for many years—the viral load and CD4 cells in the body remains relatively constant. A balance is established between the body's own defences and virus production. Most people do not show any symptoms during this phase. However, indicator conditions can occur.
This refers to conditions that indicate (the doctor says: are indicators) that a person's immune system may be weakened by an HIV infection. Such conditions include, for example, herpes zoster (shingles) or a fungal infection in the mouth and throat. Severe weight loss and/or chronic diarrhoea without an identifiable cause can also be indicators of HIV infection.
If such indicator conditions are present, doctors should offer an HIV test. The earlier an HIV infection is detected, the sooner one can begin HIV treatment and thus continue leading a normal life, even with HIV.

Late phase/AIDS:
During this phase, the viral load in the blood increases sharply again if the infection is not treated. The immune system is weakened and the HIV viruses can now multiply almost unhindered, destroying more and more immune cells. As a result, the number of CD4 cells continues to drop.
Due to the weakening immune system, other infections, which can be managed by a healthy immune system, are diagnosed. These are called opportunistic infections. When the CD4 count drops to very low levels and opportunistic infections are present, this phase is termed as AIDS or AIDS-defining illness.
HIV itself is not a disease, but a virus that infects the immune system. If left untreated, it will lead to AIDS in most cases. The abbreviation "AIDS:" stands for Acquired immune defficiency syndrome. AIDS occurs when, as a result of advanced HIV infection, the immune system is so weakened by a decrease in CD4 cells (below 200 cells/µL) that opportunistic infections can occur because the immune system is no longer able to independently fight off pathogens such as bacteria, fungi or viruses that enter the body. In this late stage of HIV infection, life-threatening illnesses often occur, such as severe pneumonia.
So, people ith HIV do not become ill immediately. Nevertheless, suitable treatment should be initiated as soon as possible after the diagnosis. The immune system can then continue to work normally to fight off pathogens and infections, just like in someone who HIV negative. This also reduces the chronic inflammation in the body that accompanies an untreated HIV infection.
If an HIV infection is treated early with appropriate medication, the development of AIDS and other consequences can be prevented. If treatment succeeds in reducing the number of viruses in the blood (the doctor speaks of “viral load") to such an extent that viruses are no longer detectable using conventional methods, an HIV-positive patient can no longer transmit the infection to others.3,4
People with HIV can now lead fulfilling and happy lives and, thanks to modern treatment options, have a life expectancy similar to people without HIV5.
FACTS AND FIGURES ABOUT HIV
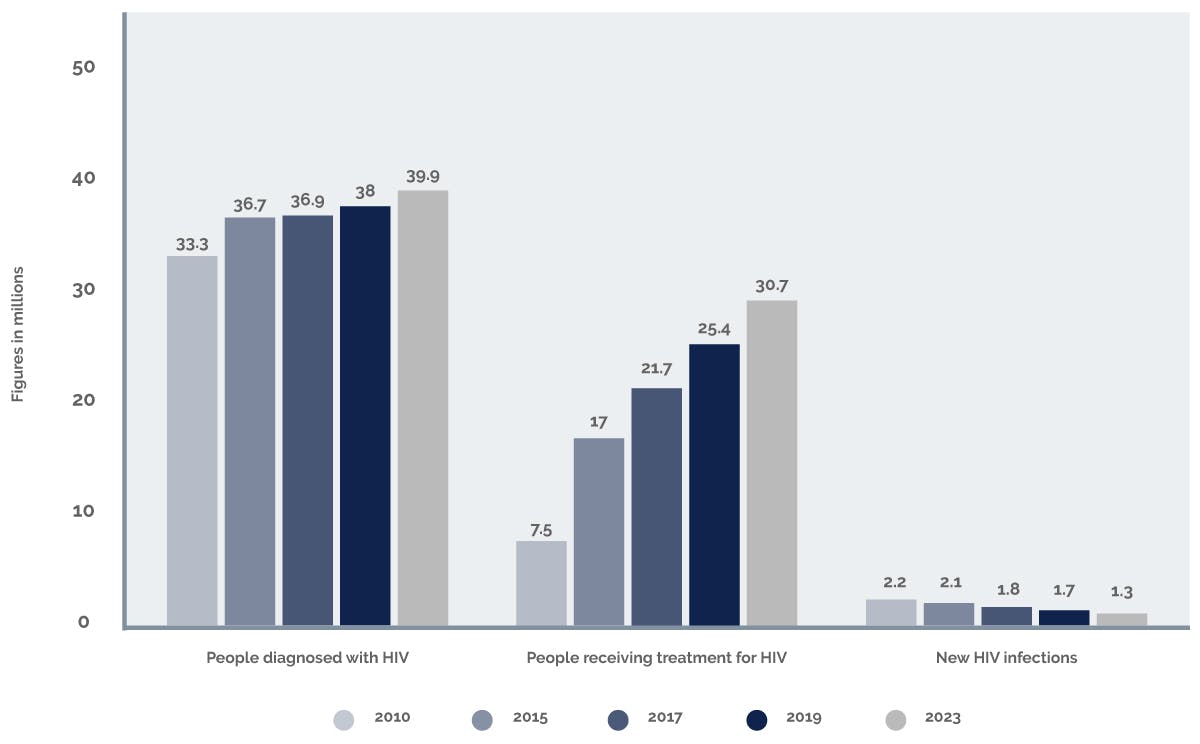
HIV through the years
The number of new HIV infections has been declining for many years – both worldwide and in Germany. Nevertheless, the total number of people living with HIV continues to rise steadily worldwide. The difference is that HIV, like many other chronic diseases, is now treatable. People with HIV who take their HIV treatment regularly to achieve an undetectable viral load, rarely develop AIDS.
As a rule, people who receive successful HIV treatment can now lead a completely normal life: they can love, have sex, work and have children – without having to fear transmitting the disease to others. (u=u)
In principle, anyone can acquire HIV, regardless of age, gender or sexual orientation. There are people all over the world living with HIV. While the Robert Koch Institute (RKI) estimates6 that the majority of people living with HIV in Germany in 2023 will be men (around 80% of people diagnosed with HIV) , women will be in the majority worldwide. According to figures collected by the United Nations Programme on HIV/AIDS (UNAIDS), approximately 39.9 million people worldwide were living with HIV in 2023. Of these, an estimated 86% know about their infection, while 14% do not.7 The proportion of people with AIDS has been steadily decreasing for many years.
Situation in Germany
According to estimates by the Robert Koch Institute (RKI), the number of people with an HIV infection in Germany6 will be 96,700 by the end of 2023. A total of 80% of them are men and 20% are women. Of these 96,700 people, the RKI estimates that around 8,200 people do not know their HIV status. However, there is also good news: in Germany, the number of new infections has been relatively constant since around 2006. In 2023, it was estimated at 2,200 people. For comparison: in the mid-1980s, the number of new infections was more than twice as high. In addition, by 2023, 96% of people diagnosed receiving treatment also had an undetectable viral load.
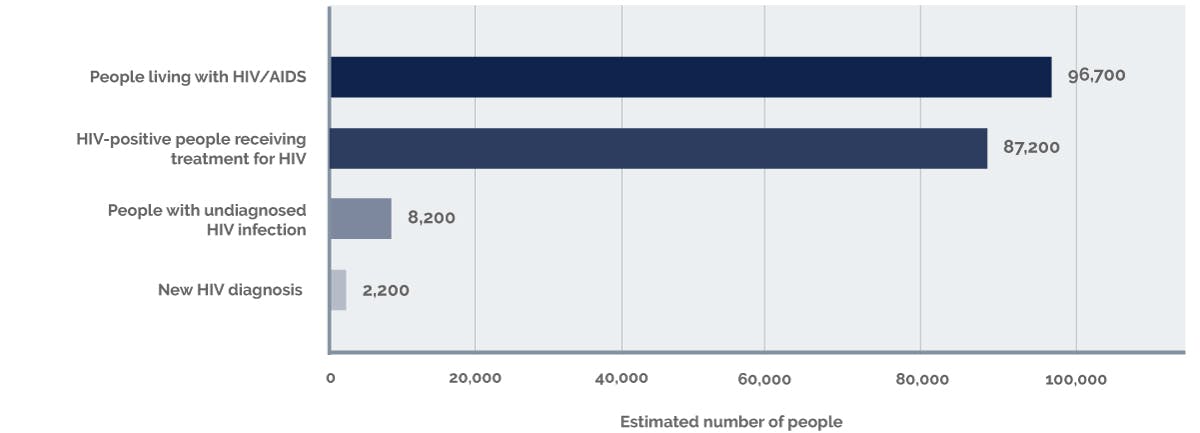
Image: Germany-wide distribution of HIV (based on figures from the Robert Koch Institute for 20236)
References:
- Schmid S, Nature Communications December 2018. https://www.nature.com/articles/d42859-018-00003-x.
- Rowland-Jones SL. Timeline: AIDS pathogenesis: what have two decades of research taught us? Nat Rev Immunol 2003 Apr; 3(4): 343–348.
- Eisinger RW et al. HIV Viral Load and Transmissibility of HIV Infection: Undetectable Equals Untransmittable. JAMA 2019 Feb 5; 321(5): 451–452.
- Leitlinien der European AIDS Clinical Society (EACS), Version 12.0, last updated October 2023. https://www.eacsociety.org/guidelines/eacs-guidelines/eacs-guidelines.html.
- Trickey et al. Survival of HIV-positive patients starting antiretroviral therapy between 1996 and 2013: a collaborative analysis of cohort studies. Lancet 2017; 4: e349–356
- Epidemiological Bulletin of the Robert Koch Institute No. 28 from 11.07.2024. https://www.rki.de/DE/Content/Infekt/EpidBull/Archiv/2024/Ausgaben/28_24.pdf?__blob=publicationFile
- UNAIDS. Global HIV Statistics. https://www.unaids.org/en/resources/fact-sheet
- https://de.statista.com/statistik/daten/studie/72727/umfrage/hiv-infizierte-und-neue-hiv-infektionen-weltweit.
NP-DE-HVU-WCNT-250003 – February 2025